Written + Fact Checked by Dr. Bardha Citaku.
Insomnia, a prevalent sleep disorder, has emerged as a silent epidemic with profound implications for society. Insomnia represents a significant public health concern, affecting millions of individuals across various demographics, notably including veterans. As a medical doctor and sleep scientist, I’ve seen firsthand how pervasive this condition is, especially among veterans who face a higher risk compared to the general population. Among its victims was Ryan Larkin, a U.S. Navy SEAL, whose struggle against insomnia caused his tragic decision to end his life. Through my work, I’ve come to understand that Cognitive Behavioral Therapy for Insomnia (CBT-I) is more than just a promising treatment for sleepless nights. It’s a journey towards comprehensive healing, addressing not only the surface symptoms but also the deep psychological scars left by trauma.
Despite its wide-reaching impact, insomnia often remains underdiagnosed and undertreated. This oversight leaves many individuals without the support they need, perpetuating the cycle of sleeplessness and its associated problems. Recognizing and addressing insomnia, particularly among high-risk groups like veterans, is crucial to mitigating its effects and improving overall public health.
In my professional experience with sleep disorders, I’ve seen how rooted in evidence-based practice, CBT-I offers a personalized approach to the multifaceted nature of insomnia, administered by trained mental health professionals. Our focus is on modifying behaviors and thought patterns related to sleep, thereby equipping individuals with practical tools to improve their sleep quality and duration.
This therapy has shown remarkable success in various populations, particularly among veterans, a group I have closely worked with. It goes beyond treating the symptoms of insomnia, addressing its underlying causes — a crucial aspect for those who have endured trauma. Through CBT-I, we aim to provide not just a treatment, but a pathway towards a significantly better quality of life for those struggling with insomnia, empowering them to make sustainable changes.
5 Key Strategies of CBT-I: Revolutionizing Insomnia Treatment
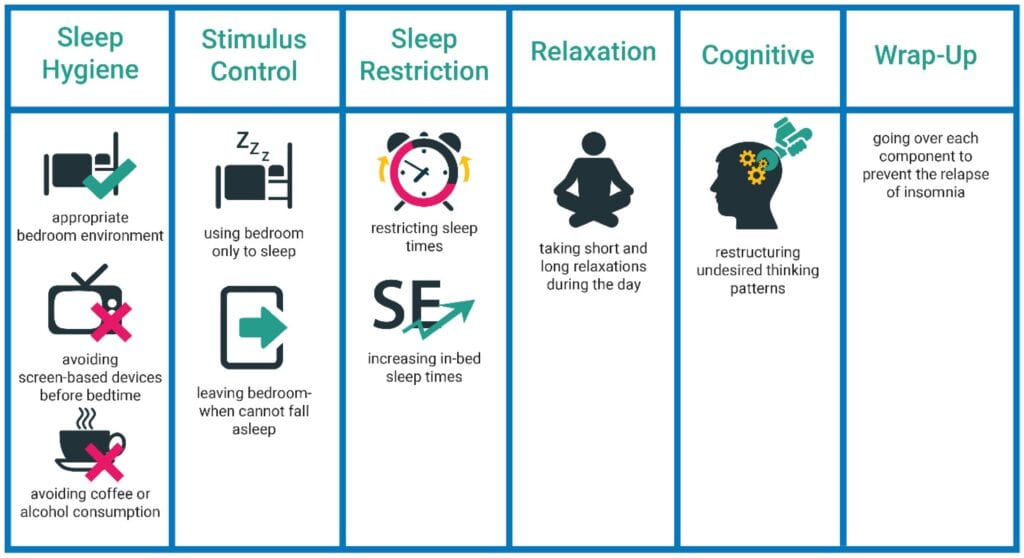
- Stimulus Control Instructions: This technique is designed to break negative associations with the bedroom environment. It involves using the bed only for sleep and sexual activity, thus reinforcing the bed as a cue for sleep rather than wakefulness. Patients are also advised to leave the bedroom if unable to fall asleep within a reasonable time, only returning when feeling sleepy
- Sleep Restriction Therapy: This method reduces the time spent in bed to the actual amount of time spent sleeping, thereby intensifying sleep drive and decreasing wakefulness at night. Over time, the time in bed is gradually increased as sleep efficiency improves.
- Cognitive Therapy: Central to addressing the psychological aspects of insomnia, cognitive therapy focuses on identifying and challenging negative thoughts and beliefs about sleep. These can include misconceptions about the consequences of poor sleep or unrealistic sleep expectations, which can increase anxiety and hinder sleep.
- Relaxation Techniques: These methods, such as progressive muscle relaxation and deep breathing exercises, are employed to reduce the physical symptoms of anxiety and create a state of relaxation conducive to sleep.
- Sleep Hygiene Education: It involves teaching about behaviors that can improve sleep quality, like maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime.
By using these techniques, CBT-I effectively dissolves the bad habits and thought patterns that contribute to insomnia. It helps people to modify their sleep environment and behaviors, address misconceptions and anxieties about sleep, and develop healthier sleep habits. This holistic treatment approach directly targets both its behavioral and psychological dimensions.
- The Effect of CBT-I on Veterans with Insomnia
Recent studies have further illuminated the effectiveness of Cognitive Behavioral Therapy for Insomnia (CBT-I) in treating veterans, a group particularly vulnerable to chronic insomnia and its debilitating effects. This new evidence strengthens the case for CBT-I as a first-line treatment for insomnia, especially for those who have served in the military. The recent findings underscore the importance of a veteran-centric approach in treating insomnia.
CBT-I’s adaptability, whether through traditional in-person sessions or innovative telehealth formats, offers hope and effective solutions for veterans struggling with sleep disturbances. These studies not only reinforce the efficacy of CBT-I in improving sleep parameters among veterans but also highlight the importance of understanding their unique experiences and challenges. By integrating these insights, we can continue to refine and enhance the delivery of CBT-I, ensuring it remains a vital and accessible tool for veterans on their journey to better sleep and overall well-being.
- Integrating Veterans' Perspectives in CBT-I
Understanding and integrating the unique experiences of veterans into the CBT-I framework is crucial. A qualitative study by Bramoweth et al. (2020), published in “Psychological Services,” emphasized the importance of considering veterans’ perspectives on insomnia treatment. The study revealed key insights into veterans’ understanding of insomnia and their preferences for care, highlighting the need for awareness and tailored approaches in delivering CBT-I to this population (Bramoweth et al., 2020).
In memory of Ryan Larkin and his battle with insomnia, our team at 62 Romeo, including myself (Bardha Citaku MD), Psychiatrist Gaurav Mishra MD, and sleep scientist Robert Sweetman, embarked on a mission to aid veterans in their fight against insomnia. As a direct participant in this groundbreaking research, I’ve witnessed firsthand the transformative impact of Cognitive Behavioral Therapy for Insomnia (CBT-I) on those who have served the country.
This initiative, deeply rooted in the principles of CBT-I, adopted an innovative approach by conducting group therapy sessions specifically tailored for veterans. These sessions, accommodating groups of 10-15 individuals, not only made CBT-I more accessible but also fostered a sense of community among participants who shared similar experiences. As a co-author of this pilot study, I can attest to the dedication and comprehensive approach our team at 62 Romeo took to address the unique challenges faced by veterans.
Our pilot study findings were significant and personally gratifying. Veterans who joined the program experienced notable improvements in their sleep patterns. After six weeks of group CBT-I therapy, which I had the privilege to co-facilitate, participants showed a marked decrease in sleep onset latency, alongside increases in both deep sleep and REM sleep. A follow-up six months post-therapy, which our team closely monitored, revealed that these improvements had persisted, demonstrating the lasting impact of CBT-I.
This experience, combined with my ongoing work in the sector, has reinforced my belief in the effectiveness of CBT-I as a transformative tool for treating insomnia. It’s not just a clinical observation but a reality I’ve seen unfold in the lives of those who have bravely served their nation.
- A Holistic Approach vs. A Quick Fix
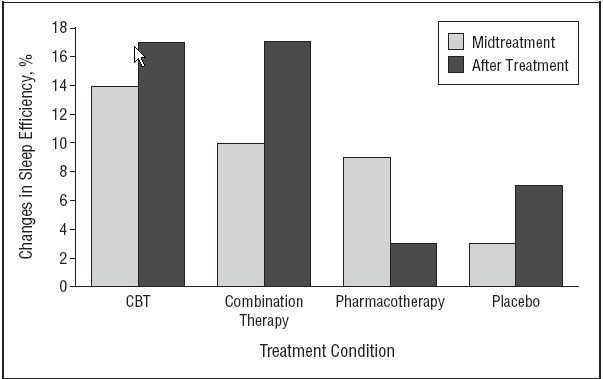
In comparison to pharmacological treatments, CBT-I stands out for its long-lasting and holistic benefits. While medications like benzodiazepines and non-benzodiazepine hypnotics can offer quick symptom relief, they often come with drawbacks such as daytime drowsiness, dizziness, and the risk of addiction. Conversely, CBT-I, devoid of these pharmacological side effects, provides a sustainable and comprehensive solution. The skills and strategies learned in CBT-I enable patients to manage their sleep independently, enhancing their overall well-being.
This approach, particularly through the lens of the veterans’ initiative, underscores the potential of CBT-I not just as a treatment for insomnia but as a tool for long-term wellness. It addresses the root causes of sleep disturbances, offering more than just symptomatic relief.
Why Is Accessing CBT-I a Challenge for Many
The implementation of Cognitive Behavioral Therapy for Insomnia (CBT-I) confronts several significant challenges that can hinder its accessibility and effectiveness.
- Shortage of Trained Therapists There’s a stark imbalance between the demand for CBT-I and the availability of trained therapists. This shortage results in long waiting times and limited access, particularly in regions without specialized providers. Addressing this gap requires enhanced training programs and incentives to encourage more professionals to specialize in CBT-I and also implementing group programs similar to ours to reach more people in need.
- Patient Adherence and Commitment
CBT-I’s efficacy hinges on the patient’s commitment to changing established sleep habits and thought patterns. The rigor of practices like sleep restriction and maintaining sleep diaries can be challenging for some, leading to decreased adherence and treatment efficacy. Developing more patient-centered approaches and providing continuous support can improve adherence rates. - Lack of Awareness and Misconceptions
A significant barrier to CBT-I’s wider adoption is the lack of awareness among both patients and healthcare providers, coupled with misconceptions about its effectiveness. Raising awareness through education and debunking myths about insomnia treatments can lead to increased utilization and acceptance of CBT-I. - Insurance and Cost Barriers The lack of insurance coverage for CBT-I poses a financial challenge for many patients. The therapy can be costly when paid out-of-pocket, limiting access for those who cannot afford it. Advocacy for broader insurance coverage and the development of more cost-effective delivery models, like digital platforms, can make CBT-I more accessible.
- Cultural and Language barriers Cultural differences and language barriers can impact the effectiveness of CBT-I, especially in diverse populations. Tailoring therapy to be culturally sensitive and available in multiple languages can enhance its efficacy and reach.
Maximizing CBT-I's potential as a first-line treatment for insomnia by addressing these challenges ensures it reaches a broader and more diverse patient population.
Dr. Bardha Citaku
Conclusion
CBT-I stands out as a highly effective treatment for insomnia, addressing both the behavioral and psychological dimensions of the disorder. Numerous studies have shown significant improvements in sleep quality, duration, and overall sleep health, evidencing the success of CBT-I. This conclusion is not solely based on academic observation, but rather on extensive hands-on experience and numerous corroborating studies. Unlike medication, which often provides temporary relief with potential side effects, CBT-I offers a sustainable, long-term solution that equips individuals with the skills to manage their sleep independently. More than just alleviating symptoms, CBT-I fosters a deeper understanding of sleep mechanisms, making it a preferred choice for my patients and many others seeking a holistic approach to overcoming insomnia. This personal journey in the world of sleep medicine has reinforced my belief in the power of CBT-I as a transformative tool in sleep therapy.
Maximizing CBT-I’s potential as a first-line treatment for insomnia by addressing these challenges ensures it reaches a broader and more diverse patient population.
References
- Cognitive Behavioral Therapy for Insomnia https://stanfordhealthcare.org/medical-treatments/c/cognitive-behavioral-therapy-insomnia/procedures.html
- Walker J, Muench A, Perlis ML, Vargas I. Cognitive Behavioral Therapy for Insomnia (CBT-I): A Primer. Klin Spec Psihol. 2022;11(2):123-137. doi:10.17759/cpse.2022110208.Rossman J. Cognitive-Behavioral Therapy for Insomnia: An Effective and Underutilized Treatment for Insomnia. Am J Lifestyle Med. 2019;13(6):544-547. Published 2019 Aug 12. doi:10.1177/1559827619867677
- Theppornpitak W, Hemrungrojn S, Thienwiwatnukul K, Muntham D, Chirakalwasan N, Srisawart P. Effectiveness of internet-based CBT-I for the treatment of chronic subthreshold to moderate insomnia. Front Neurol. 2023;14:1180339. Published 2023 Jun 2. doi:10.3389/fneur.2023.1180339
- Vedaa Ø, Kallestad H, Scott J, et al. Effects of digital cognitive behavioural therapy for insomnia on insomnia severity: a large-scale randomised controlled trial. Lancet Digit Health. 2020;2(8):e397-e406. doi:10.1016/S2589-7500(20)30135-7
- Theppornpitak W, Hemrungrojn S, Thienwiwatnukul K, Muntham D, Chirakalwasan N, Srisawart P. Effectiveness of internet-based CBT-I for the treatment of chronic subthreshold to moderate insomnia. Front Neurol. 2023;14:1180339. Published 2023 Jun 2. doi:10.3389/fneur.2023.1180339
- Bramoweth, A., Rodriguez, K., Klima, G., Appelt, C., & Chinman, M. (2020). Veterans’ experiences with and perspectives on insomnia treatment: A qualitative study.. Psychological services. https://doi.org/10.1037/ser0000494.